Blog: Pressure points
Published on 19 February 2020
Matthew McClelland, Director of Fitness to Practise, talks about how we're improving the way we take contextual factors into account and why it's important to be open with us and speak up locally about concerns
The media headlines on continuing pressures paint a sobering picture of the impact being felt by people working in and receiving health and care services.
We know some professionals are fearful that this could result in their PIN being at risk. Through this blog, I’d like to share our work on how we’re improving the way we take context into account, why it’s important to be open with us and speak up locally about concerns, and how leaders can support professionals to do this.
Everyone has a role to play
As the independent regulator for nursing and midwifery professionals practising in different health and care settings across all four countries of the UK, we don’t govern how organisations are run or how the staffing rotas for nurses, midwives and nursing associates are made up.
But we do realise that nurses, midwives and nursing associates work in multi-disciplinary teams and it’s vital they work together when working under pressure to enable the best and safest care for people. With this in mind, it’s important that we also work together with other professional regulators in this way, as demonstrated by the collaborative relationships we have with them.
Through our regulatory roles – setting standards, quality assuring education programmes, and acting fairly when fitness to practise concerns are raised – we can help influence improvement in safer care and better outcomes for the benefit of everyone involved.
In line with the Code, nursing and midwifery professionals should always put the safety of people in their care first. When working in a system under pressure, it’s more important than ever that professionals work together and use their professional judgment to assess risk and find the best way to provide care for people.
One way registered nurses, midwives and nursing associates can do this is by working effectively with colleagues across all disciplines, practising in line with the best available evidence, and recognising and working within the limits of their competence.
There are many great examples of how teams are putting this into practice. For example, Health Boards in Scotland have had success in introducing ‘safety huddles’, a forum for teams to review quality, safety, staffing levels, patient flow and other issues that may cause pressure in the system. This helps them identify risks early and work together to manage them.
Of course, there may be situations where teams are not working together well, or where professionals feel pressured to work in ways that are unsafe. In these cases, an important part of professional responsibility is to speak up.
Steps to take
The first step if you have concerns about a situation in your workplace is to raise these with your manager or senior colleague as soon as you can. If you’re not sure who to speak to, your employer should have a raising concerns policy that outlines who you can go to.
If you don’t feel able to speak to your manager or don’t feel like your concerns have been listened to, there are other ways to get support and guidance. Our raising concerns guidance for nursing and midwifery professionals is a good starting point and there are some further links at the end of this blog.
Speaking up
The publication of the NHS staff survey results for England yesterday was a clear reminder that there’s more to do to create a culture in health and social care where people feel safe and supported to speak up and have confidence that their concerns will be listened to and acted on.
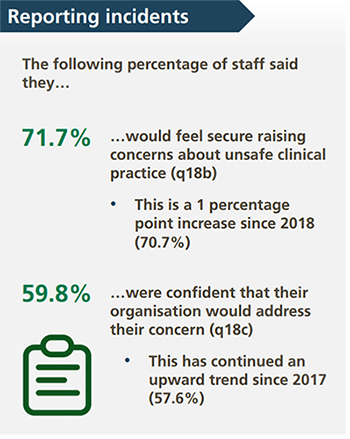
Image credit: NHS staff survey 2019
These findings are also reflected in the Paterson Inquiry, published this month, which like the Gosport Inquiry and the Mid Staffordshire Inquiry before it, highlighted how vitally important it is for professionals to speak up – and how difficult it is to do, especially if the workplace culture doesn’t encourage it.
There are signs of positive change in this area. Last month the National Guardian’s Office in England published the findings of their yearly survey of Freedom to Speak Up Guardians – individuals working in healthcare settings who are available to support colleagues to raise concerns. More Guardians than ever feel that their role is making a difference, and there’s a clear link between those organisations that support a positive speaking up culture and high quality care, with positive perceptions of the culture highest in those organisations rated good or outstanding by the Care Quality Commission.
The value of having independent sources of support and advice for people raising concerns is gaining recognition across the UK. Some Health Boards in Wales – including Cardiff and Vale – have appointed Guardians, and new processes for raising concerns in Scotland are currently being developed by the Scottish Public Services Ombudsman (SPSO).
What happens if I’m referred to the NMC?
The vast majority of nursing and midwifery professionals practise safely and effectively and will never be referred to the NMC. Each year we receive fewer than 8 referrals for every 1,000 people on our register. We recognise that being referred to us can be a daunting experience and we’re working hard to improve the way we do things. We recently launched a Careline that ensures professionals referred to the NMC have an independent place to go for emotional support if they need it.
The strategic approach to fitness to practise we adopted last year commits us to fostering a just culture in health and social care. A key focus is to improve the way we identify and take account of the context when things go wrong.
When an employer makes a referral to us, we always ask whether the nursing or midwifery professional has previously raised patient safety concerns in their organisation. That gives us an opportunity to explore whether someone might have been referred to us as a response to having raised concerns.
The use of context
We always take into account any information we have about the circumstances that have led to something going wrong and encourage professionals to be open with us about what happened and what they’ve done to put things right. That gives us the best opportunity to assess whether there’s anything more we need to do to keep people safe.
We’re working on getting even better at taking account of context. At our Open Council meeting in January, we had a fascinating and thought-provoking presentation highlighting all we’ve been doing and learning through the development and piloting of a new online tool and methodology.
We recognise that contextual factors when working under pressure – such as an undermining culture, long shift patterns, inadequate resources and a fear of raising concerns about unsafe clinical practice or negative behaviour – at best cause worry amongst professionals about the potential for punitive regulatory action. At worst, they can hinder the ability of professionals to deliver good, safe effective quality care that they aspire to.
We want to understand the whole story, not just a part of it. If we can better understand the context then we can be better able to identify whether there is a fitness to practise concern at all or whether actually the issue would be better dealt with by systems regulators.
Sources of support for raising concerns
UK-wide
- Protect is a national charity that provides a confidential advice and support line for people who have concerns about risks in the workplace.
- If you are a member of a union, you can also speak to your local representative and access advice from their guidance and helplines.
- The Royal College of Nursing has developed guidance on raising concerns for professionals working in all areas of health and care.
England
- The organisation you work for may have a Freedom to Speak Up Guardian - this is a person who is available to support colleagues to speak up when they feel unable to do so by other routes. You can look up your local Freedom to Speak Up Guardian and contact them directly.
- You can also call the Speak Up helpline – it’s free and confidential.
Northern Ireland
- The Royal College of Nursing Northern Ireland has a guide to the raising concerns process and specific guidance for nurses working in the independent sector.
- The Regulation and Quality Improvement Authority has guidance to help professionals who are considering making a protected disclosure about their concerns.
Scotland
- New processes for raising concerns in Scotland are currently being developed with the Scottish Public Services Ombudsman (SPSO ), in line with the Health and Care (Staffing) (Scotland) Act. In the meantime, professionals can follow existing advice from the Scottish Government.
- Healthcare Improvement Scotland has guidance on how NHS staff can raise patient safety concerns.
Wales
- Healthcare Inspectorate Wales has guidance for health and care professionals in Wales on raising concerns.
Other recent news…
Blog: Implementing Martha’s Rule in nursing and midwifery care: why it matters
Published on 09 September 2024
As plans to roll out Martha’s Rule continue in England, Executive Nurse Director at the NMC, Sam Foster, explains the significance of Martha’s Rule and how it r
Blog: #FutureCommunityNurse: making the most of this opportunity
Published on 05 July 2021
Our Chief Executive and Registrar, Andrea Sutcliffe, explains why your involvement in our consultation on draft standards for community and public health nursin
Blog: What we’re doing to improve how we regulate, for the benefit of the people we serve
Published on 02 June 2021
In her latest blog, Andrea Sutcliffe, our Chief Executive and Registrar, explains what we’re doing to improve how we regulate, for the benefit of the people we






