The best midwifery care happens in partnership
Every woman, baby and family should experience the best possible care during pregnancy, birth and postnatally. And as a registered midwife, you make this a reality.
Listening to and working in partnership with the women in your care is key to the person-centred midwifery care that every person has the right to expect.
Case studies
The stories of Sabina, Simone, Sophie, Josie and Sophie show us how strong partnerships with their midwives made a huge difference. You may want to reflect on these experiences, and how they might influence your own practice.
 Sabina was anxious about giving birth. She’d arranged a planned caesarean but when she developed high blood pressure and the baby needed to be delivered early, this naturally added to her concerns.
Sabina was anxious about giving birth. She’d arranged a planned caesarean but when she developed high blood pressure and the baby needed to be delivered early, this naturally added to her concerns.
But her partnership with her midwife – and particularly her midwife’s friendly and compassionate approach - helped to reassure her and her husband.
“She went out of her way to get to know us. It put us at ease.”
Early in her pregnancy, Sabina’s midwife supported her in her views and preferences for the birth despite the fears and concerns she was sharing.
“It was my first baby so I didn’t know what to expect but my midwife was very friendly and talked me through what would happen. My first scans were fantastic, seeing my baby and hearing the heartbeat.
“When I got to about 25 weeks I asked if I could have a C-section because I was terrified of giving birth. They made sure I understood my choices and the process and risks involved. I explained about my anxiety, and it gave me peace of mind knowing they’ve listened to me and supported me. They made me aware of potential consequences, but it was my choice.”
When Sabina developed high blood pressure and had to go into hospital early, the partnership that the midwife developed with Sabina, and her knowledge, listening and communication skills, helped to reassure Sabina that she could do this:
“Unfortunately, towards the end of the pregnancy I got high blood pressure and they had to bring the baby out early.
“My husband brought my bag, and we spent a full day in the ward waiting. But at about 17:00 the doctor came and apologised, saying they weren’t able to fit me in today.
Although Sabina was feeling anxious, her midwife remained calm and compassionate throughout. She continuously reassured her and explained what would happen:
“It was stressful, but the midwife was lovely and so supportive while we were waiting. She was friendly and chatty and went out of her way to speak to us and get to know us. We felt like we knew her a bit, too – that she wasn’t a total stranger. I felt a connection with her and that she was excited for us.
“She was calm and reassuring, answering our questions and helping us to understand what would happen. It made us both feel at ease. She brought us sandwiches and drinks - she knew I hadn’t eaten all day and she went and made some toast for me.
“The next afternoon they called me in to perform the C-section. Because we had a connection, she asked her supervisor if she could be the midwife to come in with us for the birth which made me feel less anxious.
“The next thing you knew our little baby boy was born. And our friendly midwife was the first one to hold him, which was really nice.”
 Through the pregnancies and births of her three children, Simone found she could rely on her midwives to support her with compassion and expert advice.
Through the pregnancies and births of her three children, Simone found she could rely on her midwives to support her with compassion and expert advice.
“I always felt they were happy to see me and hear how things were going. I never felt like I was a burden.”
For Simone, the meeting to discuss her birth plan gave her confidence in her care. It was important to see her choices and preferences were listened to and accurately recorded, and correctly followed when the time came.
“The support was definitely there even though I saw different people for the pregnancy, the birth and then the after-care.
“When it came to talking about your birth plan and what you would like, they listened, they wrote it down and it was communicated correctly so when it came to the birth, they knew everything I wanted.
“It was particularly important to feel listened to at that time.”
She was able to share her experience of miscarriage and her anxieties and her midwife responded to reassure her.
“Because I’d suffered a miscarriage previously, it was good to be able to express what had happened, to my midwife. I could really talk to her about the anxieties I had and she was able to reassure me. She made it clear they were contactable for any concerns.
“You do feel that you have a support system.”
During her first pregnancy, Simone discovered she was Group B Strep (GBS) positive1. When she became very concerned by what she read online, her midwife responded to her concerns with understanding and compassion.
“My midwife explained the different procedure we would follow for the birth - to minimise the risk of infection I would go into hospital sooner and be put on antibiotics – so that was very reassuring.
“Her care was very apparent. When she explained how we would be looked after it was calming – after everything I’d read on the internet.”
Throughout her experiences of pregnancy and birth, Simone’s midwives acted in partnership with her.
“It wasn’t a ticklist of what they need to do and send you on your way – it was very much a two-way conversation.
“They always made me feel at ease. Always asked if I had any questions. There was never any pressure on me to make a decision there and then – they always suggested I could talk with my husband and we would decide at the next session.
“All of my kids were overdue and my midwives understood the frustration and did their best to raise my spirits. They empathised with me and their comforting words just made the whole process more pleasant.”
After the birth, Simone’s midwives continued to ensure she knew to expect that she would move from the birthing suite but would have some time first with her husband and baby.
“The midwives were really good in the after-care, letting me know they would have to move me [to the postnatal ward] but giving us all that time in the birthing centre before moving, really helped the bonding time.”
“My care throughout has been great with every midwife I came into contact with.”
To hear more about Simone's story see our webinar below
References
 After the stillbirth of her first child, Sophie felt very anxious in her second pregnancy. Her midwife listened to Sophie’s history, anticipated her needs and advocated for her with the consultant and other midwives, showing compassion and leadership throughout.
After the stillbirth of her first child, Sophie felt very anxious in her second pregnancy. Her midwife listened to Sophie’s history, anticipated her needs and advocated for her with the consultant and other midwives, showing compassion and leadership throughout.
“She was fantastic at listening. The consistency of care from her, and the many small things she arranged – that I hadn’t known I needed – made me feel much more reassured.”
From the outset, her midwife established a supportive relationship. She explained she would be there for Sophie and she would not have to repeat her history to numerous different healthcare professionals.
“From that first call I was breathing a sigh of relief because of how she sounded. And it was as she said - I only ever saw her.”
At every stage, Sophie’s midwife discussed her care with her and responded to her need to take things step by step. She arranged fortnightly appointments to monitor her baby and also involved Sophie’s husband.
“We talked through anything I might need and she asked what I thought. It was always a conversation and working together.
“We were both very anxious. I couldn’t imagine getting to the end, and bringing a baby home. I essentially worked on getting to the next appointment. I never visualised the end and my midwife never pushed me to think too far ahead but helped me to focus on the next appointment.”
As the pregnancy progressed, Sophie’s midwife showed leadership in effectively communicating her needs to her consultant and other midwives. When Sophie’s concerns increased, she arranged for additional monitoring.
“She spoke to the other midwives on the assessment ward so they knew my history. When I turned up all I had to say was “I’m Sophie, I’m coming for monitoring” and they would say ‘Come in, sit down, take as long as you want’”.
When questions from staff who were unaware of her history made Sophie feel uncomfortable, her midwife placed a rainbow sticker on the front of her notes so anyone looking at her file would instantly know to be sensitive.
“The question ‘Is this your first?’ came up a lot. I’d lost my first and you don’t want to share that with everyone. Just having that little sticker on the front of my notes stopped all those uncomfortable questions. It meant a huge deal to me.”*
Sophie planned to have a caesarean and her midwife arranged for the surgical team to meet her beforehand so they would be familiar faces on the day. Following the birth, she arranged post-natal support, and also checked on Sophie a couple of months later.
“The pregnancy was very anxiety-ridden but the reassurance she gave was exactly what I needed.
“She made what was a really difficult nine months a lot easier than it would have been if she wasn’t my midwife.”
 Josie faced a difficult decision as to what type of birth to choose for her second baby. She’d needed surgery after her first baby and her recovery took several months.
Josie faced a difficult decision as to what type of birth to choose for her second baby. She’d needed surgery after her first baby and her recovery took several months.
“My midwife was neutral and didn’t push me in any direction.”
It was Josie’s partnership with her midwife – and the clear, neutral information she provided, tailored to her needs – that helped Josie make an informed choice about what to do.
Josie’s first baby weighed 10 lbs. When she discovered her second baby was also measuring large, she found herself with a difficult dilemma:
“With my first baby, I’d done a lot of research and preparation. I always think of it as a very positive labour and I was really proud. But I needed surgery afterwards and it took me a long time to recover.”
“Two years later, my second baby measured a normal size at the 20-week scan and I thought ‘Fabulous, we’ll try again for a vaginal birth’. But as time went on, my bump got bigger and bigger.
“My midwife was neutral and explained how I could go for a vaginal birth despite needing surgery the first time, and we could minimise the chance of that happening again. I realised I had a big decision to make, and I wavered back and forth.
Josie’s midwife recognised she needed to see detailed data as she considered her options. She provided Josie with the support and information she needed to be able to make her own informed decision:
“My midwife put me in touch with a birth options midwife specialist who listened to my dilemma. She was neutral and didn’t push me in any direction. She also told me I could change my mind at any point.
“I’m a Maths teacher so statistics and numbers really helped me to understand and make my decision. My midwife talked through the information with me and gave me leaflets I could study. She also sent me information about how my previous surgery might affect me.
Josie was able to come to her own decision about her birth choice because her midwives listened to her preferences and provided a neutral space as well as the detailed information she required:
“It was so important that my midwife was neutral. She understood I wanted the most information I could get, to help me make my decision.
“After taking in all that information and considering what could happen, at 38 weeks I decided to have a planned C-section.
“Both my midwife and specialist supported it fully. And he came out at 10.1lbs at 39 weeks. It was completely the right option for me. I’m so grateful that it was fully my decision.”
 Sophie had her heart set on a homebirth after weighing up her options with her midwife. Because of staff shortages it wasn’t meant to be - but thanks to her midwife’s efforts, she was still delighted with her experience in hospital.
Sophie had her heart set on a homebirth after weighing up her options with her midwife. Because of staff shortages it wasn’t meant to be - but thanks to her midwife’s efforts, she was still delighted with her experience in hospital.
“My midwife always made me feel like I was the most important person.”
Her midwife followed Sophie’s birth plan as closely as possible and then continued that partnership as she supported Sophie with initiating breastfeeding. Sophie felt listened to and reassured throughout the birth and the postnatal period.
Sophie’s midwife gave her all the information she needed to decide on a homebirth:
“My midwife visited and assessed the environment. She shared information on the benefits and risks to help me make an informed decision, and was really supportive of my choice.”
But when Sophie went into labour the homebirth service wasn’t available due to staff shortages. Her midwife thought of ways to give her some of her home comforts, releasing some of her anxiety and helping her feel good overall about the birth:
“She read my every detail of my birth plan and followed that beautifully. She listened to my preferences and where she could, got me things I would have had access to on the birthing unit – bringing me a ball, for example.
“I had wanted a ‘hands off’ approach and she was there enough but not too much.
“She gave me encouragement and reassurance when I needed it. Never having done this before, it was so important to have words of affirmation and to be told what was happening.”
In partnership with her midwife, she quickly got the hang of breastfeeding:
“As it was my first baby, I wanted to try to breastfeed but I didn’t know how. One of the midwives helped me – showing me different positions and how to make sure the latch was correct. Every time I asked for help, they were there and supported me.
“I vividly remember my day five check, and my baby had gained weight. I can still remember the midwife saying to me ‘This is amazing, you’re doing the right things, whatever you’re doing keep doing it’. I remember walking out of there with a spring in my step thinking “OK, I’ve got this.”
Feeling listened to provided Sophie with a reassuring and positive experience.
“They must have been attending to many other women on the ward but it never felt like that. Despite how busy they must have been they always made me feel like I was the most important person at that time.”
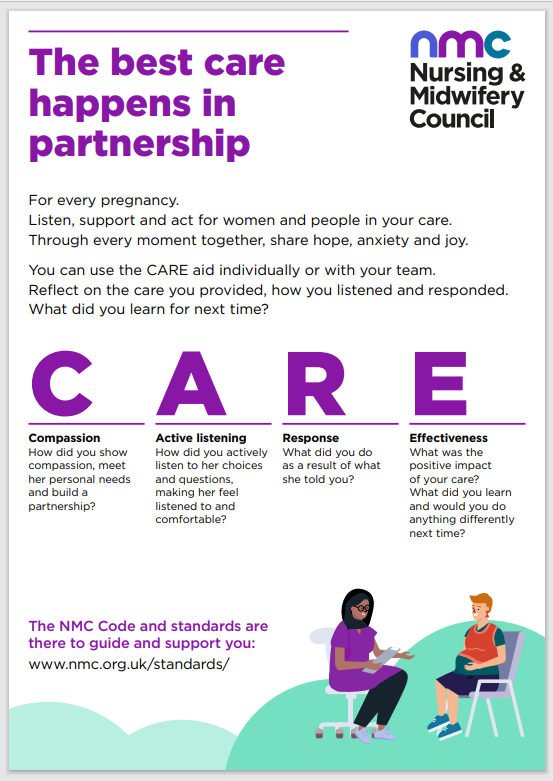
CARE reflective aid
Our Code and standards of proficiency are here to help you reflect on the importance of listening and working in partnership.
To support your individual and group reflection, try our midwifery CARE reflective aid.
It highlights how Compassion, Active listening, Response and Effectiveness are at the heart of care. The prompts can support all midwives to reflect on how to apply the standards in their day-to-day practice.
The CARE reflective aid can be downloaded and printed for easy reference. You can also use this aid during your revalidation.
Webinar
In this webinar, you’ll hear from two women who have recently given birth about how strong partnerships with their midwives made a huge difference to how they felt about the care they experienced. And our senior midwifery advisers, Verena Wallace and Jacqui Williams, explore what our standards say about the importance of good listening and partnership.
For the women in your care: what they can expect
 We’ve also developed a campaign intended for women in antenatal care, to empower them in their part of the partnership with you: For Every Pregnancy.
We’ve also developed a campaign intended for women in antenatal care, to empower them in their part of the partnership with you: For Every Pregnancy.
Sharing these materials could help you set the tone and make the women in your care feel at ease. Why not put up the poster in your waiting room?