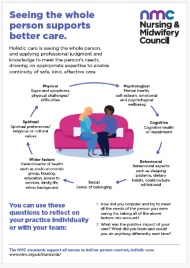
Holistic care
There is so much more to a person than the personal health goal, or illness or condition, they’re being treated for. Who they are as an individual does so much to determine their health and care journey. This includes aspects such as mental and physical health, spiritual beliefs, cognitive health and behavioural elements, as well as social and personal circumstances.
As a nurse, you see the whole person, and apply your professional judgement and knowledge to meet their needs, drawing on expertise from other fields of practice as appropriate.
You ensure the continuity of safe, kind, effective care is truly person-centred.
Case studies
How does thinking holistically help nurses deliver better care for people? Read the experiences of nurses from different fields of practice and the people they've cared for, sharing the positive impact of holistic care.
 Tracy Cox, a Consultant Learning Disability Nurse for Community Therapeutic Services, and Craig, an individual she’s supported, discuss their experiences and views of holistic care.
Tracy Cox, a Consultant Learning Disability Nurse for Community Therapeutic Services, and Craig, an individual she’s supported, discuss their experiences and views of holistic care.
Tracy has a passion for supporting people with a learning disability and with additional complex challenging and mental health needs. In Tracy’s view, working in partnership is essential to delivering holistic care:
“Working in partnership with the individuals you’re supporting but also with families and other professionals, is paramount. Shared decision making is key, and being open to listening to others and making sure they have a voice, because you learn from others as well.”
“It’s important to be clear about specific roles and responsibilities, and to reflect, and share experiences.”
For Tracy, advocating for the people in her care has been the most important aspect of holistic care:
“The biggest thing for me in working with Craig and others with learning disabilities, is being able to advocate for them if they’re not able to advocate for themselves – making sure we are their voice and making sure they get the right support at the right time from the right people.”
She considers nurses would benefit from connecting and working together more, to help share ideas about delivering the best possible care:
“I don’t know if it’s the length and breadth of my time as a nurse but I think sometimes people don’t connect enough with each other, and don’t network with each other enough. I think we need to be comfortable with drawing on each other. It’s reciprocal – I know so many people I can ask for help”
Craig has a learning disability and spent 11 years in hospital under section under the Mental Health Act. Now supported to live in the community, he describes the care he has received on coming out of hospital, and the ways nurses have taken into account all of his needs – practical, emotional, psychological, physical and mental, as well as medical care:
“There were two student nurses who were very helpful, helping me budget, buying food and helping me make food independently. My community nurse helped me moving out of hospital and moving into my new place. He used to take me out for coffees, have a chat how I’m getting on, and helping me with problem-solving.
“He took me to the doctors to get my bloods done now I’m a lot better as I’ve been taking my meds, and that’s important.
Craig explains how feeling listened to built trust and helped him to feel safe and confident:
“It’s good when other people listen to you because it makes you more safe, and makes you confident.
“I trust Tracy and it’s good to trust people but that’s if they treat you well and you get used to them. Then you express your feelings to somebody who you know will listen and talk to you. “
For Craig to attend essential health appointments, for example at the dentist, psychological support has been key.
“We’ve been meeting the Learning Disability Liaison nurse from the hospital for coffees – just to get used to her.
“We chat about anything, play games with her - I’m the best at Connect 4. And she shows me around the hospital.
“We’re taking it really slowly, next time I see her I’ll go into the dental hospital, just for a look at my mouth, nothing else.”
Tracy explains how taking things slowly, at Craig’s pace, has helped him with looking after his teeth:
“What we’ve been doing is taking it very slowly. It’s called ‘De-sensitisation’– taking it slowly to introduce Craig to the place and to gradually get to know it.
Also, we sent over his health passport so they have it on their system and every time you go in, they know about Craig.
Tracy explains how Craig’s care has supported him to live safely out of hospital and in the community, by considering his views, and taking all of his needs into account:
“We were talking about what we consider to be the most important aspect – for it to be person-centred and for Craig to always have a voice, and for people to listen to his wishes even if they’re not what is considered the right decision - and we have to respect that.
Tracy Cox is a Consultant Learning Disability Nurse for Community Therapeutic Services (now retired), with a passion for supporting people with a learning disability with additional complex challenging and mental health needs. Tracy worked within the NHS for 30 years where she led the Intensive Response Team in Bristol before working as a Community Services Manager for the Learning Disabilities service for Avon and Wiltshire Partnership Trust. She is now working part time for NHS Bristol, North Somerset and South Gloucestershire completing a piece of work related to Section 117 aftercare.
 Caroline Ogunsola is Professional Development Lead Nurse for Community & Primary Care Services at East London NHS Foundation Trust. She is passionate about community nursing as an opportunity to go further to deliver holistic care in the home.
Caroline Ogunsola is Professional Development Lead Nurse for Community & Primary Care Services at East London NHS Foundation Trust. She is passionate about community nursing as an opportunity to go further to deliver holistic care in the home.
Caroline sees taking a holistic approach to care as key to empowering nurses to do more for the people they care for.
“I believe nurses should focus on delivering holistic care for people because it allows us to look at the entirety of the person and their being. It empowers us to do more for them.
“With a holistic approach, nurses are able to consider aspects of the person’s well-being such as their spirituality, social connections, how things are with them generally – as well as assess whether medication is working.
“It’s a privilege to be able to spend time with people and talk to them about how they are feeling. As a nurse, our skill is to use our conversations to understand what really matters to the person. If we listen, they will tell us how they feel their care should be delivered.
Seeing people in their own home really helps nurses to deliver holistic care in the community.
“Community nursing is my passion, I believe in seeing a person in their own environment because this plays a big part in who, and what they are. I love going into people’s homes – you are able to do a lot for them and provide what they need to make them more comfortable.
“Delivering care in a person’s own home will help their health and well-being because they are in their own environment, and they have control.”
For Caroline, a holistic approach brings people’s’ own knowledge and understanding of themselves, into the delivery of their care.
“For me, care should be co-produced with the person you’re caring for. It’s not the case that as a nurse you know it all. The person can also contribute and, working with their nurse, learn to manage their condition. For example, a person with chronic obstructive pulmonary disease (COPD) may not need to see their GP so often if they know their exacerbation points and are able to control their COPD with the help of their nurse.
“Holistic care also raises the profile of nurses as a profession to people. Surveys show people have high trust in nurses so it’s important that we build on that and show we trust them and their knowledge, too, and work with them.”
Caroline thinks nurses have a unique ability to apply their knowledge when planning and delivering care.
“Being a nurse means often being with the person we’re caring for more than other healthcare colleagues. This gives us the opportunity to learn about them and gain a sound understanding of how we can support them. This enables nurses to share what we’ve observed, consider potential scenarios and suggest the options most likely to help.
“Bringing what we know about the person together with our theoretical knowledge helps our professional judgement.
“As a nurse, we use all the information we gather to coproduce, plan and deliver care with the person we’re caring for.”
She believes the Code gives clear guidance for nurses delivering holistic care
“Holistic care is at the heart of the Code. Considering how we apply this in our practice can help guide us to develop our clinical judgement.
“Boundaries are also an important area for those of us who are privileged to go into people’s homes, and to have conversations onwards. Some people are vulnerable, and we must ensure we safeguard and protect them so they feel comfortable when they see us.”
In Caroline’s view, a holistic approach helps give people ownership of their care.
“The great advantage of holistic care to people is they have a say in what is happening, and can take a lead in what is being delivered to them. The person is at the heart of it all, they can feel confident they have the power to manage their health day to day, supported by their carers and family.
“Giving people ownership of their care helps their recovery.”
Caroline Ogunsola is professional development lead nurse for community services, and lead for non-medical prescribing at East London NHS Foundation Trust. She is a Clinical Fellow at NHS England, is a Queen’s Nurse, and holds a Master of Science (MSc) in Education.
 Lauren Pinnell is a trainee advanced clinical practitioner in the Health in Justice sector as a clinical lead for new models of care. She is leading an approach to enable people to fully access integrated person-centred healthcare.
Lauren Pinnell is a trainee advanced clinical practitioner in the Health in Justice sector as a clinical lead for new models of care. She is leading an approach to enable people to fully access integrated person-centred healthcare.
“Working with prison teams, we’ve moved away from the traditional model where teams or specialities work in siloes. We’re rolling out an integrated healthcare approach that follows the individuals’ journey.
“We have multidisciplinary teams (MDT) working under the banners of ‘Early Days in Custody’, ‘Planned Care’ and ‘Unscheduled Care’. These teams are composed of a range of specialities or skillsets such as mental health nurses, adult nurses, substance misuse specialists, medical practitioners, paramedics, physiotherapists, and also administrators.”
Lauren believes people have better outcomes from care that integrates multiple skillsets.
“As an example of a ‘physical health’ emergency that led to the person receiving holistic care: our Unscheduled Care Team attended a ‘code blue’ emergency when a person had been released from a ligature by prison officers. There was an immediate assessment for physical harm before the attending mental health nurse assessed their mental health care needs.
“The multidisciplinary team were able to look at the person through each of the speciality lenses but also agreed a care plan swiftly. This provided the person and the team the opportunity to be involved in the decision-making process.
“Having a joint planning approach enabled the team to move from a reactive to a more flexible, proactive response and help prevent the person going into crisis again”.
In Lauren’s view, shared decision-making is the most important advantage of a holistic approach.
“We can’t be masters of all trades – and people will respond to different approaches. We need to understand and appreciate everyone’s skillset or the lens they are looking through. Involving a colleague with the right specialism is only going to help our own collaborative decision making.
“For example, a person may be refusing their ‘psychotropic’ medication, with implications for their health. A mental health nurse may have a more detailed understanding of this type of medication and might be better placed to support the person to make an informed decision and enable the MDT to develop their knowledge around this particular intervention”.
Lauren thinks seeing the person first, and looking at them holistically enables safe, kind and effective care.
“One of the key things about our integrated approach is a culture of learning, and empowering people to use their clinical curiosity to gather as much information as we can so we can use it to plan care and to support the person.
“Core to our approach is to start care planning from the moment a person comes in. Starting by looking at them as a whole and identifying their healthcare needs, being able to plan and put interventions in place sooner, leading to better outcomes.”
Lauren sees the strength of a holistic approach in acknowledging the role of the individual to improve their own health outcomes.
“I truly believe in looking at the person holistically from the start, it enables us to make every opportunity count. People within prisons are very vulnerable and often their life ‘on the outside’ is not supportive for their health outcomes. We hope investing time in them through a holistic approach and encouraging them to be responsible for their own health, will better support them for when they get out.”
Lauren Pinnell is London Regional Primary Care and NMOC Clinical Lead working in the Health in Justice sector as a clinical lead for new models of care.

 Professor Linda Ross, University of South Wales, and Professor Wilfred McSherry, Staffordshire University, are leading research and education on spiritual care in nursing and midwifery. They developed the Spiritual Care Education Standard that is now part of the pre-registration nursing curriculum in Wales.
Professor Linda Ross, University of South Wales, and Professor Wilfred McSherry, Staffordshire University, are leading research and education on spiritual care in nursing and midwifery. They developed the Spiritual Care Education Standard that is now part of the pre-registration nursing curriculum in Wales.
Linda explains that spirituality refers to people’s beliefs and values, the things that give them purpose and meaning – which may or may not be religious.
“Spiritual care is about a person’s sense of connection and what’s most meaningful for them. For some it’s their religious belief but for others it may be their loved ones, or connection to nature. For anyone we care for, it’s that same principle of finding out what’s important to them and creating a connection.”
She describes how spirituality has a positive impact on person-centred care.
“You can use your conversation in a therapeutic way to bring healing and open up an opportunity for the person to say what’s on their mind, and important to them.
“There’s an example of a nurse caring for a man after a stroke, who used photos on his bedside table to prompt a conversation about hiking and connecting with nature. This broke down barriers and helped her understand what was important to him.
“The impact for him was huge. And when reflecting on this the nurse was able to be positive about this experience as she had understood his needs, what was important to him and the struggles he faced – and how that was impacting on his recovery.”
For Wilf, a critical incident early in his career led him to study the impact of people’s values and beliefs on their care needs.
“As a newly qualified nurse, I was helping a man to get ready to be discharged after blood tests had ruled out a heart attack or myocardial infarction. I had given him his outdoor clothing but moments later, he collapsed and was under the care of the resuscitation team when his wife arrived to collect him. She was very concerned, repeatedly asking to see her husband but he died before this could happen. In distress, his wife asked, “Where’s the priest?” but nothing had been recorded as to his beliefs, which I then had to clarify with her. I still see that lady leaving the ward – that afternoon is as clear today as when it happened”.
“That was the driving force for me to prevent anything like that happening again. I went back to university to look at the impact of people’s beliefs on their care needs and spirituality started coming into focus.”
For both Linda and Wilf, early experiences in nursing demonstrated the transformational potential of spiritual care and shaped their careers. Linda describes the experience that led to 30 years in research and publishing on spirituality:
“I was caring for an elderly woman who was bed-bound, unable to speak or eat, her days spent staring at a wall. I felt she had no quality of life so when I found an old bible while tidying her locker, I asked if she would like me to read to her. Her eyes lit up, and I can still see her face today.
“Seeing that transformation, I realised there’s got to be more to caring for people than expert physical care.”
Wilf explains how being guided by the individual they’re caring for can give nurses and midwives confidence to address spirituality.
“Sometimes there’s anxiety about spiritual care. If you are always guided by the person you’re caring for so you don’t do anything unless it’s what they or their family or main carers have expressed, you won’t go wrong because you are addressing something they feel is important to them. It’s about expressed need.”
Wilf sees nurses and midwives as uniquely placed to deliver spiritual, holistic care.
“Other colleagues look to us to advocate holistic care in a meaningful way. If we don’t, it diminishes the impact of the nurse and midwife because holistic care is so important.”
“There’s no care without spiritual care –those values and connections, everything that’s dear to people are important.”
Linda explains that person-centred spiritual care applies to all aspects of life and care.
“Our beliefs, values and so on are challenged by any life-changing event, positive or negative. Spiritual care starts in compassionate relationship and moves in whatever direction need requires. It’s that art of being directed by people’s need.
“When people understand what it’s about, they absolutely get it – this is core to our humanity.”
Linda describes the model of spiritual care developed to help professionals in everyday practice, called The 2 Question Spiritual Assessment Model (2QSAM).
“These are two really simple questions anyone can use to start a person-centred, holistic dialogue: ‘What’s most important to you right now?’ and ‘How can we help?’.
“If you use these questions during every care moment, it allows spiritual care to be directed by the person and their needs. It also means you’re addressing whatever is most important at that point in time.
“It helps keep the person you’re caring for and their current need at the forefront, and allows the nurse to be comfortable in the care they’re providing.”
Linda Ross is Professor of Nursing (Spirituality) at the University of South Wales, Visiting Professor at Staffordshire University and a Fellow of AdvanceHE (formerly The Higher Education Academy). She was the first person to explore nurses’ perceptions of spirituality and spiritual care. Today she works with partners to shape spiritual care in nurse/midwifery education in the UK and Europe in her roles as Chair, All Wales Spirituality, Health and Wellbeing Special Interest Group, Founding member and Chair of the EPICC Network and Director, Trustee, Founding member of the International Network for the Study of Spirituality and Co-Editor in Chief of its ‘Journal for the Study of Spirituality’, among others.
Wilf McSherry is Professor in Nursing working in the Department of Nursing, School of Health, Education, Policing and Sciences, Staffordshire University. Wilf is a founding and executive member of the International Network for the Study of Spirituality, a Principal Fellow of AdvanceHE (and Fellow of the Royal College of Nursing. He was Lead Partner for the European project titled Enhancing Nurses Competence in Providing Spiritual Care through Innovation Education and Compassionate Care (EPICC) and is a steering group member of the recently established EPICC Network.
Reflective aid
 Our Code and standards of proficiency are here to help you reflect on the importance of holistic care.
Our Code and standards of proficiency are here to help you reflect on the importance of holistic care.
To support your individual and group reflection, try our holistic care reflective aid.
It highlights how seeing the whole person is core to care in nursing. The prompts can support all nurses to reflect on how to apply the standards in their day-to-day practice.
The aid can be downloaded and printed for easy reference. You can also use this aid during your revalidation.
The NMC standards support all nurses to deliver person-centred, holistic care.






